We examined the relationship between SBP and DBP with the risk of BC in a large population-based cohort study. We found that DBP was associated with an increased risk of BC for postmenopausal women, independently of previous diagnoses of hypertension. We observed a strong positive association of DBP values over 85 mmHg with BC, particularly in the range of 85 to 89 mmHg among postmenopausal women. This finding agrees with a study where DBP over 85 mmHg was associated with BC risk in a population of American postmenopausal women7. Similarly, a recent study using the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort reported a positive association of both SBP and DBP categorized by the American Hypertension Association (AHA) and the European Society of Hypertension with BC risk in postmenopausal but not in premenopausal women6. In contrast to our results, this European study reported a significant increase of 3% BC risk per 10 mmHg increase in SBP and DBP and a positive dose response among BP categories. These differences might be explained by population characteristics and genetic heterogeneity between population studies18. A study from Norway, Austria and Sweden reported an increased BC risk for the highest quintile values of SBP and DBP for all women8. Conversely, a prospective study from Australia found no association between BP measurements and BC risk9. However, in a secondary analysis, DBP between baseline and the second follow-up wave were associated with triple negative breast cancer risk. While the SBP associations in previous studies are conflicting, our study did not find an association between SBP and BC risk, presumably due to dissimilarities in population characteristics and BP cutoff ascertainment. Furthermore, similar to previous pooled cohort studies4,5, we found that hypertension, defined as self-reported combined with objectively measured blood pressure, is positive associated with BC risk.
These epidemiological findings must be put in context of the physiopathology of hypertension and breast cancer. The physiological link between high BP and cancer risk is still unclear. One main issue about BP parameters is that while age is positively correlated with SBP increase, DBP is not as straightforward. SBP increases continuously with age, whereas DBP increases until the fifth decade and then slowly decreases from the sixth decade due to vascular stiffness as part of the normal aging process19. DBP has two major components: peripheral vascular resistance (PVR) and artery compliance20,21. PVR is the total resistance to blood flow across the vascular system determined by the small arterioles. Artery compliance refers to the distensibility of the blood vessels due to blood volume, a term which is related to the elasticity of blood vessels22. If PVR and artery compliance increase, then DBP would increase. However, aging reduces artery compliance and/or increases artery stiffness, decreasing DBP19. Even though there is evidence suggesting that both peripheral (muscular) and central (elastic) arteries in hypertensive individuals are stiffer compared to normotensive individuals, in individuals with isolated hypertension, where the SBP is increased with a normal DBP value, the stiffness is increased in large aortic but not peripheral arteries23,24. Hence, increased DBP values might negatively affect blood flow fluctuations in the peripheral vessels affecting organs like the breast.
In addition to age, other factors increase BP, including decreased baroreceptor and chemoreceptor sensitivity, increased responsiveness to sympathetic nervous system stimuli, altered sodium metabolism, and altered renin-angiotensin metabolism. Additionally, after menopause, women lose estrogen-vascular protection25. The decrease in endogenous estrogens, mediated by estrogen receptors (ERs), leads to endothelial vasoconstriction, increasing peripheral vascular resistance26,27,28,29. Therefore, lower estrogen levels in blood might also contribute to lower arterial compliance and increased risk of high BP in postmenopausal women30,31,32.
Thus, slight alterations in the arterial lumen, either functional or structural, result in significant changes in arterial resistance. Moreover, menopause has been shown to accelerate age-related rises in sympathetic nerve activity (SNA), related to impaired central modulation of baroreflex function and direct inhibitory influence of estrogen on SNA33. The increased activity of SNA increases the PVD, increasing BP. However, whether menopause or estrogen have a larger effect on DBP than SBP has not been reported to the best of our knowledge. It is possible that with altered central autonomic regulation coupled with enhanced vascular adrenergic sensitivity may be responsible for elevated DBP and exaggerated pressor responses to exercise and mental stress in some postmenopausal women33,34.
In postmenopausal women, local adipose tissue increases and stroma tissue diminishes in the breast. Adipose cells in breast tissue produce estradiol locally from circulating precursors35. Therefore, estradiol levels are higher in breast tissue than in the bloodstream, especially in postmenopausal women36,37. Genotoxic metabolites from estradiol contribute to BC development38. Hence, high local estrogen production and altered blood flow in breast tissue may contribute to chronic local inflammation, cell proliferation stimulation, and tumor micro-environment enhancement39. Therefore, we propose that increased DBP might not be a causal risk factor for BC, but it might be an important contributor to BC development in postmenopausal women. In this context, postmenopausal women with less-aged vessels in the breast area due to local increased estrogen production accompanied by altered high blood flow in the peripheral vessels are more likely to experience BC (Fig. 2). Although, SBP has been associated with breast cancer in other studies6, SBP is more related to the cardiac stroke volume than the PVR. Therefore, as PVR increases, SBP will also increase but not as much as DBP40,41. On contrary, in premenopausal women, no association between BP and BC risk might be partially explained by the estrogen’s vascular protective factors in this period26,27,42.
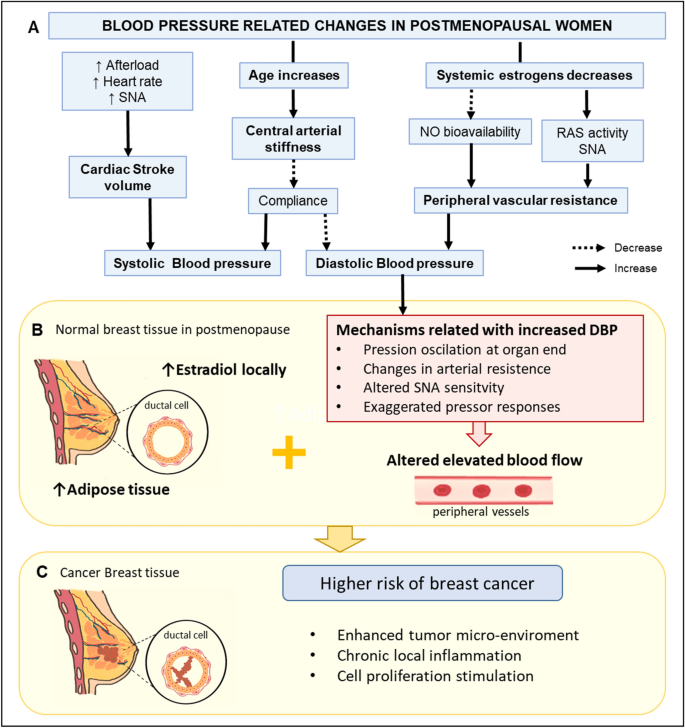
Putative mechanism related to DBP and increased risk of breast cancer in postmenopausal women. (A) Physiological responses for an increase in age and decrease in systemic estrogens and their influence on the SBP and DBP. (B) Hypothetical mechanisms related to increased DBP and altered blood flow and its association with increased estrogen production in breast cancer tissue. (C) Local estradiol and altered blood flood in breast tissue could enhance tumor microenvironment, local inflammation, and cell proliferation stimulation, increasing breast cancer risk. NO nitric oxide, RAS renin-angiotensin system, SNA sympathetic nerve activity, SBP systolic blood pressure, DBP diastolic blood pressure. The figure was generated using Microsoft PowerPoint (2016) and Sketchbook (iOS version 5.2.2).
High BP, a consequence of the interaction of genetic and environmental factors, causes oxidative stress resulting in smooth muscle hypertrophy and spasm, endothelial dysfunction, subendothelial low density lipoprotein deposition and oxidation in the vascular walls43,44. Similarly, breast cancer may be attributed to oxidative stress in old age where protein damage, DNA damage, and lipid peroxidation may increase the BC risk independently45,46. Proposed biological mechanisms for explaining the link between high BP and BC include chronic inflammation process, modification in apoptosis activation, and disequilibrium in the renin-angiotensin system47,48,49,50,51,52, which might be related to BP components, but further research is needed. Recently an in-vitro study showed that G protein coupled receptor kinase 4 (GRK4), a regulator of renal sodium excretion, functions as an independent proliferation promotor in BC cells53. Furthermore, evidence suggests that controlling BP may reduce the risk of BC54. Although the evidence is still contradictory and associated to specific antihypertensive drugs54,55, the positive association between hypertension and BC risk disappeared when treated vs. untreated hypertension was evaluated in a large European cohort study6.
Being overweight or obese has been related to breast cancer risk56 and hypertension57. We analyzed the association of DBP and breast cancer risk by BMI subgroups and found no interaction, which means that the effect of DBP on breast cancer risk is independent of women BMI.
This study has some limitations. First, there is a lack of information on changes over time for BP measurements and some potential confounding self-reported variables, which may result in misclassification bias. Although our models were adjusted for the use of HRT, we lack information on the type and duration of HRT which may affect the association in postmenopausal women. Furthermore, we lack information on the type of hypertension treatment or antihypertensive drug used in hypertensive individuals which may have reduced the strength of hypertension associated with breast cancer. Also self-reported hypertension might be misleading due to measurement error or recall bias. Additionally, only one measured hypertensive value is not enough for hypertension diagnosis. Therefore, combining both methods might improve the underestimation of a hypertension diagnosis in the “healthy” population. Hence, we included self-reported hypertension diagnosis as a confounding variable in our third model, aiming to control both the antihypertensive treatment and the length of the hypertension diagnosis58. Also, the secondary analyses excluding hypertensive individuals showed that previous hypertension diagnosis did not affect the association of normal-high DBP values and BC incidence.
One of the challenges of working with BP measurements is classification. The criteria used to define BP cut-offs have been changing over the last few decades depending upon different approaches. We selected the cut-offs of the 2020 International Society Hypertension guidelines as our categorization criteria due to their recent publication, worldwide use, and tailored use in low and high resources settings15. Additionally, as this population-based cohort includes mainly “healthy participants”, we analyzed BP using binary cut-offs at the normal category for DBP and SBP to increase the statistical power for the higher BP groups.
Despite the limitations, the strengths of our study include its prospective study design in a large cohort, the availability of objectively measured SBP and DBP by trained staff and the high accuracy of BC diagnoses retrieved from the KCCR. This study is the first in our knowledge to examine the association of BP measurements and BC risk in an Asian large-based population cohort. Moreover, the number of participants and BC cases were similar among premenopausal and postmenopausal women, which allows us to draw conclusions. However, we cannot exclude the possible misclassification of perimenopausal women. Additionally, detailed information of established risk factors for breast cancer such as reproductive factors, family history of BC, smoking, and lifestyle risk factors was available, enabling adjustment for potential confounders.
In summary, this study suggests that normal-high DBP values are associated with increased BC risk in postmenopausal women. We propose that mildly elevated DBP values are associated with an increased probability of BC, but they are not necessarily causal factors. Still, DBP could be used for the risk calculation of BC occurrence. Our observations suggest the importance of DBP to estimate BC risk, particularly in postmenopausal women. This epidemiological association still requires further research in larger samples and, ultimately, potential mechanisms involved need to be elucidated.
link






More Stories
Heart conditions and pregnancy: Know the risks
Pregnancy and COVID-19: What are the risks?
What Medications Are Safe While Breastfeeding?